These are educational slides from my lectures. i have videos of some recent lectures on my youtube channel: https://youtube.com/user/leichangmoh
李長茂Dr Clarence Lei Chang Moh
- Clarence Lei ChangMoh
- Dr Clarence Lei Chang Moh, FRCS Urol (MMC No.: 024209, NSR 123533) Adjunct Professor, Universiti Malaysia Sarawak, Honorary Consultant SGH, Heart Centre Sarawak, Hospital KL; Consultant Urologist(Adult and Paediatric), Kidney, Urology, Stone, Prostate & Transplant) Normah Hospital, Petra Jaya, 93050 Kuching, MALAYSIA Tel: +6082-440055 e-mail: clarencelei@gmail.com telemedicine welcome; email or whatsapp+60128199880; standard charges RM235 for first & RM105 subsequent
Thursday, September 1, 2011
UROLOGICAL CONDITIONS IN CHILDREN
UROLOGICAL CONDITIONS IN CHILDREN
by Dr Clarence Lei, FRCS Urol, Consultant Urologist, email: clarencelei@gmail.com
INTRODUCTION:
The scope of discussion will include the clinical presentation, the medical
treatment, the timing and a brief description of any paediatric urologic surgery required.
UROLOGICAL CONDITIONS in children include: circumcision, undescended testes (UDT),
scrotal swellings including hydrocele and hernia, acute scrotal pain incl torsion, hypospadias. A
dilated urinary tract is the commonest antenatal diagnosis and the causes include: PUJO, pelvi-
ureteric junction obstruction, VUJO, vesico-ureteric junction obstruction, VUR, vesico-ureteric
reflux and PUV, posterior urethral valve. Neuropathic bladder is also increasingly an important
cause of dilated urinary tract. Finally, urogenital tumours include those of the kidneys (Wilms),
testes and the rare rhabdomyosarcoma of the prostate.
The commonest medical indication for circumcision is phimosis, as manifested by ballooning
of the prepuce at micturation. Circumcision has also been shown to reduce the incidence of UTI,
urinary tract infection and probably viral infections (including HIV) of the male and the female
partners (later). Paraphimosis in a young boy is a surgical emergency.
The incidence of undescended testes at birth is 10% and this decreases to 1% at the age of 1 year.
Bilateral undescended testes can be occasionally treated by injection HCG. After the age of 1
year, any undescended or ectopic testes require surgery as soon as possible. Complications
include torsion and associated hernia. In adolescence, the testes can undergo malignant change.
Hence, orchidopexy and testicular self examination are important health education for testicular
maldescent. Hernia in children should always be operated as soon as possible to reduce the risk
of strangulation requiring emergency surgery. Persistent increasing hydrocele after the age of 1
year can also be operated electively via an inguinal approach so as to do a herniotomy at the same
time. I routinely drain the hydrocele as well.
Acute scrotal pain is testicular torsion unless proven otherwise. Such proof may be in the
form of diagnosis of torsion appendix testis or an inflammation as evidenced by urgent doppler
ultrasound, which can occur in 50% of children with scrotal pain.
Bilateral antenatal hydronephrosis in a male child is often due to PUV, posterior urethral valve.
Ultrasound would also indicate a distended and thickened bladder. PUV associated with sepsis
(often introduced during an MCU !) and renal impairment are best treated by a vesicostomy.
Where facilities are available including paediatric cystoscope, the PUV can then be fulgurated
with closure of the vesicostomy electively.
Bilateral hydronephrosis without renal impairment in the female and all unilateral
hydronephrosis can be treated electively. Ultrasound can be done within the first week of
delivery and functional study about 6 weeks later, when the kidneys have achieved some
maturity. The appropriate functional study for the kidneys is an isotope scan (usually Tc labeled
MAG-3) to see the differential function and the drainage of the dilated system. Many such
asymptomatic hydronephrotic system improves as the child grows older. It is realised nowadays
that only about 30% of such patients require surgery. The indications of surgery would be
increasing dilatation and deterioration of function on serial isotope scans (e.g. decreased to 30%).
The standard treatment would be an excision of obstruction and a pyeloplasty.
The current treatment for vesicoureteric reflux is to give a therapeutic dose of antibiotics
urgently when there is a febrile UTI. Long term prophylactic antibiotics and surgery is now
recognised as not improving the long term outcome. There is an increased usage of cystoscopic
Deflux injection of the ureteric orifice to reduce the incidence of febrile UTI. High grade reflux
tends to have more febrile UTI and therefore more interventions with injection therapy.
Where the urinary tract dilatation is due to a duplex system, a definitive treatment would be
surgical excision of the hydronephrotic poorly functioning duplex moiety. Neuropathic bladder
can be closely monitored with ultrasound, radio isotope study and referral for urodynamics,
if there is any deterioration. High pressure bladder can cause renal failure and such bladders
are best treated with cystoplasty (often a “clam” type) followed by CIC, clean intermittent
catheterisation. Urinary stones are occasionally seen in children and treatment is similar as
adults, namely, by ESWL, extracorporeal shockwave lithotripsy or by endourology.
Hypospadias occurs in 1 : 300 of newborns. The main aim of surgery is to enable the child to
pass urine standing up and also to have a penis straight enough for eventual sexual relations.
The recommended age for surgery is after the age of 1 year (unless the penis is very small) and
to finish surgery before the child goes to school. There are many techniques for hypospadias
surgery and most requires the patient to have some kind of catheter for at least a week. They will
often require a second stage operation.
CONCLUSION:
The medical personnel and parents should also know the common complications and
outcome of the conditions. The referral mechanism and the follow-up protocol depend on the local
facilities.
Tuesday, August 16, 2011
A speech
Good Evening, Ladies & Gentlemen;
may I have ur
A special good evening to Mr David Tolley,
President of Royal College of Surgeons, & Mrs Tolley;
Good evening also to Mr Sam McClinton, Past-President of the Scottish Urological Society n Lead Examiner, & Mrs McClinton,
This is not a formal dinner but it is still good to say a few words at an important gathering like this.
The Sarawak Club was founded in 1876 by Sir Charles Brooke, who was the second white Rajah of Sarawak.
Sarawak was a separate state by itself: in fact u may have noticed that one still need a passport to enter Sarawak !
A surgeon, Dr MacDougall founded one of the earlier hospitals in Kuching. His wife founded a famous school very near to Pullman hotel, the St Mary’s school, where my wife, Ivy Chin has been a senior teacher for > 20 years. She is also responsible for this dinner!
I went Edinburgh
NOW EDINBURGH
I want to welcome three special guests tonight: Dr John Chew, the Chairman of the Sarawak state Malaysian Medical Association & Dr Peter Wong , Secretary of the Malaysian College
Please enjoy the rest of the dinner and I hope we do meet again.
Dr Clarence Lei, clarencelei@gmail.com
Saturday, August 6, 2011
MEN'S HEALTH - ED, Erectile Dysfunctio
HOW COMMON IS ED?
Men's health has been a neglected component of community health care. There are many
programmes for the children and women; indeed many are sponsored by the State.
Erectile function is an important component of men's health and can be a strategy to
improve the provision of men's health. Erectile dysfunction or ED is defined by the
National Institute of Health, U.S.A. as the persistent inability to initiate and/or maintain
an erection of the penis sufficient to permit satisfactory sexual intercourse. The term
"ED" is referable to "Impotence" because impotence implies a hopeless situation.
According to established epidemiology surveys, at least 10% of men have ED. However,
ED can be mild, moderate or severe. This figure rises to at least 50% in special risk
groups, e.g. patients with diabetes or moderate hypertension.
WHY BOTHERS WITH ED?
In the Asian community, ED is still a taboo subject, even with doctors. It is well known
that ED impacts severely on the quality of life. The ED patient typically suffers from the
following: guilt, depression, anxiety, frustration, low self esteem. The partner may feel
rejected, thinking that the husband no longer desires her or is having an extra marital
affair.
WHAT CAUSES ED?
Although there is an inevitable psychological component with ED, most ED patients have
an underlying physical cause. Patients should not seek treatment for ED in isolation.
The underlying causes should be treated:
• Arteriosclerosis or hardening of arteries.
• Hypertension.
• Diabetes.
• Heart disease.
• Neurological disorders.
• Neurological diseases.
• Diseases of the lower urogenital tract, e.g. cancer prostate, penile deformities.
• After pelvic surgery.
• Certain medications.
WHAT LIFESTYLE CHANGES CAN YOU MAKE TO DECREASE ED?
Obviously, a healthy lifestyle contributes to many of these diseases as well as to ED
itself. This will include the following:
• Quit smoking.
• Reduce consumption of alcohol.2
• Exercise.
• Reduced obesity.
• Diet modification to reduce high cholesterol or triglycerides.
• Adequate relaxation and rest.
• Better communication with your partner.
HOW DO YOU ASSESS ED?
Depending on the severity of symptoms scored on the International Index of Erectile
Function (IIEF), ED can be classified as mild (score 12-21), moderate (score 8-11) or
severe (score 5-7). The incidence of erectile dysfunction in Malaysia has been studied by
the National Family Planning and Development Board and is very similar to the
Massachusetts Male Aging study in U.S. It is also age related. Briefly, 50% of men at 50
years of age have ED, 60% at 60 years and 70% at 70 years.
International Index of Erectile Function (IIEF)
Answer these questions if you are concerned about Erectile Dysfunction.
WHAT TESTS SHOULD BE DONE TO ASSESS ED?
In addition to a detailed medical history and physical examination (including DRE,
digital rectal examination of the prostate), certain tests can be done. The urine
examination and blood sugar assessment is usually done. If the patient also suffers from
a loss of libido (desire for sex), blood may be taken to check the hormonal profile
(namely, total testosterone and prolactin). Depending on the underlying pre-existing
medical illnesses, blood for cholesterol, kidney function, liver function may also be
tested. If the patient also has urinary symptoms, then other aspects of men's health (e.g.
urine flow rate and blood for PSA or prostatic specific antigen) may be done. In
exceptional cases, detailed evaluation may be done and this includes colour doppler study
of the blood flow to the penis and to test for nocturnal penile tumescence (NPT).
WHAT TREATMENT ARE AVAILABLE FOR ED PATIENTS?
Sildenafil (trade name, Viagra) was introduced in Malaysia in 1999 and that
revolutionised the treatment of ED. Prior to that, the main treatment for ED was to inject
a drug into the penis to cause vasodilatation and erection. If that fails, then the main
treatment was to surgically insert a penile implant. In early 2004, the patients have a
choice of two new oral medications for ED, namely, Tadalafil (trade name, Cialis) and
Vardenafil (trade name, Levitra). These drugs enhance the penile erection when a person
is sexually stimulated but the erection is not sufficient for sexual activity. Penile erection
occurs when nerve stimulation causes the release of chemicals in the penis which in turn
causes dilatation of the vessels. This group of oral medications block the breakdown of
these chemicals (called vasodilators) and therefore help to enhance the penile erection.
These drugs work only when the erection is insufficient for sexual activity and not if the
erection is normal. If the erection is already normal, the vasodilator receptors are used up
and taking these oral medications will not enhance a normal erection.
WHAT DO PATIENTS EXPECT FROM THE ORAL MEDICATIONS?
The oral medications are remarkably effective and the effectiveness range from 80% to
about 50% in more severe cases. Patients have to see their doctors to see the underlying
cause of their ED as well as to discuss treatment expectations. For those patients whose
initial treatment with oral medication fails, further tests may be necessary.
WHAT ARE THE SIDE EFFECTS OF ORAL MEDICATIONS FOR ED?
As with all medications, there are some side effects. These drugs cause increased blood
flow to the penis and to some other parts of the body as well and therefore, can cause a
drop in the blood pressure. If patients are taking a class of drugs called nitrates for chest
pain, then it is an absolute contraindication to the taking of these 3 types of oral
medications. In addition, these 3 medications cause side effects which are mostly related
to dilatation of blood vessels, namely:4
• Facial flushing.
• Indigestion.
• Backache.
• Headache.
• Nasal congestion.
• Dizziness.
The side effects are mild and transient. If they persist, this usually means that the patient
has to decrease the dosage of the oral medication. These 3 oral medications have been
proven with a high level of scientific evidence by doing double-blind placebo controlled
clinical trials to be effective. This is unlike most of the traditional medications or fake
products which are touted in the market or Internet. It is therefore important to get such
expensive medications from a quality assured outlet, e.g. Normah Medical Specialist
Centre.
HOW ARE THE MEDICATIONS TAKEN?
The 3 types of medications are taken on an as required basis. The duration of action is ½
hour to 4 hours (Viagra and Levitra) although one of them can last up to 36 hours
(Cialis). Cialis and Levitra may be taken with or without food.
SUMMARY:
Assessment and treatment for ED is an important avenue for improving men's health. For
many, treating ED is just as important as treating underlying medical illness and adopting
a healthy lifestyle.
Dr Clarence Lei Chang Moh, FRCS Urol, FEBU, FAMM
Consultant Urologist
Feb 2004
Men's health has been a neglected component of community health care. There are many
programmes for the children and women; indeed many are sponsored by the State.
Erectile function is an important component of men's health and can be a strategy to
improve the provision of men's health. Erectile dysfunction or ED is defined by the
National Institute of Health, U.S.A. as the persistent inability to initiate and/or maintain
an erection of the penis sufficient to permit satisfactory sexual intercourse. The term
"ED" is referable to "Impotence" because impotence implies a hopeless situation.
According to established epidemiology surveys, at least 10% of men have ED. However,
ED can be mild, moderate or severe. This figure rises to at least 50% in special risk
groups, e.g. patients with diabetes or moderate hypertension.
WHY BOTHERS WITH ED?
In the Asian community, ED is still a taboo subject, even with doctors. It is well known
that ED impacts severely on the quality of life. The ED patient typically suffers from the
following: guilt, depression, anxiety, frustration, low self esteem. The partner may feel
rejected, thinking that the husband no longer desires her or is having an extra marital
affair.
WHAT CAUSES ED?
Although there is an inevitable psychological component with ED, most ED patients have
an underlying physical cause. Patients should not seek treatment for ED in isolation.
The underlying causes should be treated:
• Arteriosclerosis or hardening of arteries.
• Hypertension.
• Diabetes.
• Heart disease.
• Neurological disorders.
• Neurological diseases.
• Diseases of the lower urogenital tract, e.g. cancer prostate, penile deformities.
• After pelvic surgery.
• Certain medications.
WHAT LIFESTYLE CHANGES CAN YOU MAKE TO DECREASE ED?
Obviously, a healthy lifestyle contributes to many of these diseases as well as to ED
itself. This will include the following:
• Quit smoking.
• Reduce consumption of alcohol.2
• Exercise.
• Reduced obesity.
• Diet modification to reduce high cholesterol or triglycerides.
• Adequate relaxation and rest.
• Better communication with your partner.
HOW DO YOU ASSESS ED?
Depending on the severity of symptoms scored on the International Index of Erectile
Function (IIEF), ED can be classified as mild (score 12-21), moderate (score 8-11) or
severe (score 5-7). The incidence of erectile dysfunction in Malaysia has been studied by
the National Family Planning and Development Board and is very similar to the
Massachusetts Male Aging study in U.S. It is also age related. Briefly, 50% of men at 50
years of age have ED, 60% at 60 years and 70% at 70 years.
International Index of Erectile Function (IIEF)
Answer these questions if you are concerned about Erectile Dysfunction.
WHAT TESTS SHOULD BE DONE TO ASSESS ED?
In addition to a detailed medical history and physical examination (including DRE,
digital rectal examination of the prostate), certain tests can be done. The urine
examination and blood sugar assessment is usually done. If the patient also suffers from
a loss of libido (desire for sex), blood may be taken to check the hormonal profile
(namely, total testosterone and prolactin). Depending on the underlying pre-existing
medical illnesses, blood for cholesterol, kidney function, liver function may also be
tested. If the patient also has urinary symptoms, then other aspects of men's health (e.g.
urine flow rate and blood for PSA or prostatic specific antigen) may be done. In
exceptional cases, detailed evaluation may be done and this includes colour doppler study
of the blood flow to the penis and to test for nocturnal penile tumescence (NPT).
WHAT TREATMENT ARE AVAILABLE FOR ED PATIENTS?
Sildenafil (trade name, Viagra) was introduced in Malaysia in 1999 and that
revolutionised the treatment of ED. Prior to that, the main treatment for ED was to inject
a drug into the penis to cause vasodilatation and erection. If that fails, then the main
treatment was to surgically insert a penile implant. In early 2004, the patients have a
choice of two new oral medications for ED, namely, Tadalafil (trade name, Cialis) and
Vardenafil (trade name, Levitra). These drugs enhance the penile erection when a person
is sexually stimulated but the erection is not sufficient for sexual activity. Penile erection
occurs when nerve stimulation causes the release of chemicals in the penis which in turn
causes dilatation of the vessels. This group of oral medications block the breakdown of
these chemicals (called vasodilators) and therefore help to enhance the penile erection.
These drugs work only when the erection is insufficient for sexual activity and not if the
erection is normal. If the erection is already normal, the vasodilator receptors are used up
and taking these oral medications will not enhance a normal erection.
WHAT DO PATIENTS EXPECT FROM THE ORAL MEDICATIONS?
The oral medications are remarkably effective and the effectiveness range from 80% to
about 50% in more severe cases. Patients have to see their doctors to see the underlying
cause of their ED as well as to discuss treatment expectations. For those patients whose
initial treatment with oral medication fails, further tests may be necessary.
WHAT ARE THE SIDE EFFECTS OF ORAL MEDICATIONS FOR ED?
As with all medications, there are some side effects. These drugs cause increased blood
flow to the penis and to some other parts of the body as well and therefore, can cause a
drop in the blood pressure. If patients are taking a class of drugs called nitrates for chest
pain, then it is an absolute contraindication to the taking of these 3 types of oral
medications. In addition, these 3 medications cause side effects which are mostly related
to dilatation of blood vessels, namely:4
• Facial flushing.
• Indigestion.
• Backache.
• Headache.
• Nasal congestion.
• Dizziness.
The side effects are mild and transient. If they persist, this usually means that the patient
has to decrease the dosage of the oral medication. These 3 oral medications have been
proven with a high level of scientific evidence by doing double-blind placebo controlled
clinical trials to be effective. This is unlike most of the traditional medications or fake
products which are touted in the market or Internet. It is therefore important to get such
expensive medications from a quality assured outlet, e.g. Normah Medical Specialist
Centre.
HOW ARE THE MEDICATIONS TAKEN?
The 3 types of medications are taken on an as required basis. The duration of action is ½
hour to 4 hours (Viagra and Levitra) although one of them can last up to 36 hours
(Cialis). Cialis and Levitra may be taken with or without food.
SUMMARY:
Assessment and treatment for ED is an important avenue for improving men's health. For
many, treating ED is just as important as treating underlying medical illness and adopting
a healthy lifestyle.
Dr Clarence Lei Chang Moh, FRCS Urol, FEBU, FAMM
Consultant Urologist
Feb 2004
Tuesday, August 2, 2011
Sexual and overall quality of life
The role of Alpha Blockers in BPH, sexual and overall quality of life
Lower urinary tract symptoms, LUTS related to BPH not only impair the quality of life
but also affect sexual function. The symptoms may be related to bladder outlet
obstruction or altered bladder muscle function. There are two components of obstruction
viz static and dynamic. Alpha adrenergic blocker therapy act on the dynamic component
by reducing the sympathetic tone of the prostatic urethra:
(1) irrespective of the size of the prostate gland
(2) improve the symptoms score viz IPSS by 8 points including nocturia and border
score
(3) improve the uroflow by 3 mls/s.
(4) works rapidly, within days
(5) can therefore be used before a trial off catheter in acute urinary retention.
(Alfuzosin XL 10 mg when used for 3 days, 62% have successful trial off catheter.
Alfuzosin 10 mg daily achieves its maximum dose effect without the need of titration
and on a once daily basis, improving compliance.)
(6) The effect of alpha-blockers is sustained for many years; most clinical trials are up
to 48 months. For uro-selective alpha-blockers, its systemic side effects are
minimal with 4.2% withdrawals from treatment due to side effects, the main one of
Alfuzosin is that of dizziness, 3.1%.
There is a close relation between LUTS and sexual dysfunction. This is possibly
related to the presence of PDE-5, nitride oxide, sympathetic tone of the prostate and penis
as well as similar innervation. Accordingly, 70% of patients with severe LUTS have ED.
Treatment with Alfuzosin “improves the sexual drive, decreases ED by 26%, improve
painful ejaculation in 65%”. There is a significant 30% abnormal ejaculation for patients
who are on Tamsulosin 0.8 mg versus a very low rate of 0.3% for patients on Alfuzosin.
Conversely, treatment with PDE-5 inhibitors either alone or in combination with alphablockers (which is safe) also improves LUTS. Indeed, prolonged erection or priapism has
occasionally been reported as a complication of alpha-blocker therapy.
Improvement of LUTS and sexual function from alpha-blockers without significant
adverse events & positively impact on quality of life (BPH QoL20 score improved 45%
at 36 months). This is more so when patients in this group have significant comorbidities. In the AMORE, Asian Multi-national Prospective Observational Registry of
patients with BPH, there are significant associated hypertension (43%), diabetes mellitus
(14%), IHD (10%) and obesity (36%). Treatment with Alfuzosin 10 mg daily has
marginal blood pressure changes in this group of patients, even >65 years of age and on
anti-hypertensive therapy. Alpha-blocker therapy (e.g. Alfuzosin 10 mg daily) is
efficacious in the treatment of BPH, improves sexual function and quality of life.
e-References available on request from author.
Malaysian Urological Conference Lecture on 8.12.2007
by Dr Clarence Lei Chang Moh, FRCS Urol, FEBU,
Adjunct Professor, Universiti Malaysia Sarawak
e-mail: clarencelei@gmail.com
Lower urinary tract symptoms, LUTS related to BPH not only impair the quality of life
but also affect sexual function. The symptoms may be related to bladder outlet
obstruction or altered bladder muscle function. There are two components of obstruction
viz static and dynamic. Alpha adrenergic blocker therapy act on the dynamic component
by reducing the sympathetic tone of the prostatic urethra:
(1) irrespective of the size of the prostate gland
(2) improve the symptoms score viz IPSS by 8 points including nocturia and border
score
(3) improve the uroflow by 3 mls/s.
(4) works rapidly, within days
(5) can therefore be used before a trial off catheter in acute urinary retention.
(Alfuzosin XL 10 mg when used for 3 days, 62% have successful trial off catheter.
Alfuzosin 10 mg daily achieves its maximum dose effect without the need of titration
and on a once daily basis, improving compliance.)
(6) The effect of alpha-blockers is sustained for many years; most clinical trials are up
to 48 months. For uro-selective alpha-blockers, its systemic side effects are
minimal with 4.2% withdrawals from treatment due to side effects, the main one of
Alfuzosin is that of dizziness, 3.1%.
There is a close relation between LUTS and sexual dysfunction. This is possibly
related to the presence of PDE-5, nitride oxide, sympathetic tone of the prostate and penis
as well as similar innervation. Accordingly, 70% of patients with severe LUTS have ED.
Treatment with Alfuzosin “improves the sexual drive, decreases ED by 26%, improve
painful ejaculation in 65%”. There is a significant 30% abnormal ejaculation for patients
who are on Tamsulosin 0.8 mg versus a very low rate of 0.3% for patients on Alfuzosin.
Conversely, treatment with PDE-5 inhibitors either alone or in combination with alphablockers (which is safe) also improves LUTS. Indeed, prolonged erection or priapism has
occasionally been reported as a complication of alpha-blocker therapy.
Improvement of LUTS and sexual function from alpha-blockers without significant
adverse events & positively impact on quality of life (BPH QoL20 score improved 45%
at 36 months). This is more so when patients in this group have significant comorbidities. In the AMORE, Asian Multi-national Prospective Observational Registry of
patients with BPH, there are significant associated hypertension (43%), diabetes mellitus
(14%), IHD (10%) and obesity (36%). Treatment with Alfuzosin 10 mg daily has
marginal blood pressure changes in this group of patients, even >65 years of age and on
anti-hypertensive therapy. Alpha-blocker therapy (e.g. Alfuzosin 10 mg daily) is
efficacious in the treatment of BPH, improves sexual function and quality of life.
e-References available on request from author.
Malaysian Urological Conference Lecture on 8.12.2007
by Dr Clarence Lei Chang Moh, FRCS Urol, FEBU,
Adjunct Professor, Universiti Malaysia Sarawak
e-mail: clarencelei@gmail.com
SEXUAL DYSFUNCTION OF CHRONIC ILLNESS AND MANAGEMENT
Sexual dysfunction
Sexual dysfunction affects negatively quality of life. An obvious component of sexual
dysfunction is that of erectile dysfunction, ED. ED is defined as the persistent inability
to achieve and/or maintain an erection sufficient for satisfactory sexual activity. Age is
an important risk factor for ED. Sixteen per cent of Malaysian men aged 40 – 70 years
suffers from complete ED. Management should be aimed not only at treatment but also
at prevention of ED. Despite having the first impotence clinic in GHKL in 1992, only
10% of Malaysian men with ED talked to the doctors and only 3.9% had received some
form of treatment. Sildenafil (trade name Viagra) was found to be effective amongst
Malaysians in a double blind placebo controlled study published in 2000. Even then,
Sarawakian men sought advice regarding their ED after an average duration of 20
months.
Erection is a complex neurovascular event, modified by psychological factors. The comorbidities of ED are similar to those for ischaemic heart disease and strokes. ED should
be treated as part of total wellness of the patients by family doctor, taking into account
hypertension, ischaemic heart disease, dyslipidaemia, diabetes, psychological stresses,
family factors, diet, exercise, smoking etc.
All such co-morbidities are common in chronic renal failure. In addition, chronic renal
failure is associated with hormonal imbalances involving testosterone and prolactin.
Studies of ED in chronic renal failure patients showed a prevalence of about 60% with
half of this suffering from severe ED. Dialysis patients above the age of 50 have an
almost 70% chance of having ED. In one study, it was found that the incidence of ED is
irrespective of social economic status and duration of haemodialysis. In another study,
63 out of 68 patients on peritoneal dialysis suffered from ED.
The treatment of ED has been revolutionised by the introduction of the phosphodiesterase
Type 5 inhibitor (PDE-5 I). There are 3 main PDE-5 inhibitors currently being used,
namely, Sildenafil, Vardenafil and Taladafil. These medications can be taken ½ to 1
hour before sex; the effect of Sildenafil and Vardenafil last for 4 hours and that of
Taladafil for 36 hours. They should not be taken on a full stomach. Sexual and penile
stimulation is required as PDE-5 inhibitors enhance an erection but does not induce
an erection! PDE-5 inhibitors are generally safe and the main contraindication is that
these medications should not be taken concurrently with any form of nitrates eg GTN,
Isordil, Imdur. Taking PDE-5 I together with nitrates can result in hypotension. PDE-5 I
works in about 60% of ED patients, less if the patients have numerous untreated comorbidities. The side effects of PDE-5 inhibitors include flushing, headache and nasal
congestion. Another treatment is that of intra-penile injection of a vasodilator, e.g.
Caverject 20 mcg. Over-dosage can result in prolonged erection viz priapism. Any
erection more than 4 hours should be brought down, usually with penile aspiration or
injection of a dilute vasoconstrictor gradually e.g. Phenylephrine. Other modalities
include penile rings to reduce venous leak and also vacuum pumps to increase blood flow
into the penis. Finally, for patients with “end stage penile failure, ESPF”, a penile
prosthesis can be inserted by open surgery. Many traditional therapies are available but 2
these have not been tested with double blind placebo controlled trials. Moreover, some
of these therapies (e.g. subcutaneous injections for penile lengthening) can have serious
side effects
The role of testosterone in erectile dysfunction has recently taken a more prominent role,
with the availability of long acting (3 months) injection testosterone. There is some
association of testosterone deficiency syndrome (TDS) with truncal obesity in men,
diabetes, hypertension, dyslipidaemia (metabolic syndrome).
The International Society for Sexual Medicine defines premature ejaculation as
ejaculation which occurs within 1 minute of vaginal penetration and resulting in negative
personal consequences. Premature ejaculation is probably more common than ED and
difficult to treat, especially if it is chronic. The treatment consists of physical methods
(e.g. squeeze technique) and the use of selective serotonin re-uptake inhibitors, SSRI, e.g.
Fluoxetine 20 mg 2 hours before sex.
Female sexual dysfunction (FSD) consists of impaired sexual interest (52%), orgasmic
dysfunction (19%), vaginismis (18%) and dyspareunia (4%). Female sexual arousal
disorder is defined by WHO as the persistent inability to attend or maintain sexual
excitement, express as a lack of genital lubrication or swelling response. Chronic
illnesses including diabetes mellitus double the risk of FSD especially arousal difficulties,
pain during sex and infection. Sildenafil does not treat FSD although it is postulated to
have some effect on clitoral erection and on the G-spot.
Fertility in patients with chronic illnesses is often decreased in part due to ED,
ejaculatory disorders and infection of the lower urinary & genital tract. For patients with
ejaculatory problems, sperm can be harvested by post orgasm urine or electro-ejaculation.
Sperm can also be harvested nowadays from the testes and kept in sperm bank. Modern
test tube baby techniques e.g. intracytoplasmic sperm injection (ISCI) can help many
subfertile couples.
SUMMARY:
ED is seen in about 60% of patients with chronic renal failure. Specific treatment with
PDE-5 I is effective in more than 60% of patients. ED should be treated early together
with the co-morbidities viz hypertension, diabetes, ischaemic heart disease,
dyslipidaemia, mental health and testosterone deficiency syndrome. Intra-penile
injection of vasodilators is useful in patients who do not respond to PDE-5 I.
NKF Annual Dialysis Meeting, Kuala Lumpur, 13th
December 2008
Sexual dysfunction affects negatively quality of life. An obvious component of sexual
dysfunction is that of erectile dysfunction, ED. ED is defined as the persistent inability
to achieve and/or maintain an erection sufficient for satisfactory sexual activity. Age is
an important risk factor for ED. Sixteen per cent of Malaysian men aged 40 – 70 years
suffers from complete ED. Management should be aimed not only at treatment but also
at prevention of ED. Despite having the first impotence clinic in GHKL in 1992, only
10% of Malaysian men with ED talked to the doctors and only 3.9% had received some
form of treatment. Sildenafil (trade name Viagra) was found to be effective amongst
Malaysians in a double blind placebo controlled study published in 2000. Even then,
Sarawakian men sought advice regarding their ED after an average duration of 20
months.
Erection is a complex neurovascular event, modified by psychological factors. The comorbidities of ED are similar to those for ischaemic heart disease and strokes. ED should
be treated as part of total wellness of the patients by family doctor, taking into account
hypertension, ischaemic heart disease, dyslipidaemia, diabetes, psychological stresses,
family factors, diet, exercise, smoking etc.
All such co-morbidities are common in chronic renal failure. In addition, chronic renal
failure is associated with hormonal imbalances involving testosterone and prolactin.
Studies of ED in chronic renal failure patients showed a prevalence of about 60% with
half of this suffering from severe ED. Dialysis patients above the age of 50 have an
almost 70% chance of having ED. In one study, it was found that the incidence of ED is
irrespective of social economic status and duration of haemodialysis. In another study,
63 out of 68 patients on peritoneal dialysis suffered from ED.
The treatment of ED has been revolutionised by the introduction of the phosphodiesterase
Type 5 inhibitor (PDE-5 I). There are 3 main PDE-5 inhibitors currently being used,
namely, Sildenafil, Vardenafil and Taladafil. These medications can be taken ½ to 1
hour before sex; the effect of Sildenafil and Vardenafil last for 4 hours and that of
Taladafil for 36 hours. They should not be taken on a full stomach. Sexual and penile
stimulation is required as PDE-5 inhibitors enhance an erection but does not induce
an erection! PDE-5 inhibitors are generally safe and the main contraindication is that
these medications should not be taken concurrently with any form of nitrates eg GTN,
Isordil, Imdur. Taking PDE-5 I together with nitrates can result in hypotension. PDE-5 I
works in about 60% of ED patients, less if the patients have numerous untreated comorbidities. The side effects of PDE-5 inhibitors include flushing, headache and nasal
congestion. Another treatment is that of intra-penile injection of a vasodilator, e.g.
Caverject 20 mcg. Over-dosage can result in prolonged erection viz priapism. Any
erection more than 4 hours should be brought down, usually with penile aspiration or
injection of a dilute vasoconstrictor gradually e.g. Phenylephrine. Other modalities
include penile rings to reduce venous leak and also vacuum pumps to increase blood flow
into the penis. Finally, for patients with “end stage penile failure, ESPF”, a penile
prosthesis can be inserted by open surgery. Many traditional therapies are available but 2
these have not been tested with double blind placebo controlled trials. Moreover, some
of these therapies (e.g. subcutaneous injections for penile lengthening) can have serious
side effects
The role of testosterone in erectile dysfunction has recently taken a more prominent role,
with the availability of long acting (3 months) injection testosterone. There is some
association of testosterone deficiency syndrome (TDS) with truncal obesity in men,
diabetes, hypertension, dyslipidaemia (metabolic syndrome).
The International Society for Sexual Medicine defines premature ejaculation as
ejaculation which occurs within 1 minute of vaginal penetration and resulting in negative
personal consequences. Premature ejaculation is probably more common than ED and
difficult to treat, especially if it is chronic. The treatment consists of physical methods
(e.g. squeeze technique) and the use of selective serotonin re-uptake inhibitors, SSRI, e.g.
Fluoxetine 20 mg 2 hours before sex.
Female sexual dysfunction (FSD) consists of impaired sexual interest (52%), orgasmic
dysfunction (19%), vaginismis (18%) and dyspareunia (4%). Female sexual arousal
disorder is defined by WHO as the persistent inability to attend or maintain sexual
excitement, express as a lack of genital lubrication or swelling response. Chronic
illnesses including diabetes mellitus double the risk of FSD especially arousal difficulties,
pain during sex and infection. Sildenafil does not treat FSD although it is postulated to
have some effect on clitoral erection and on the G-spot.
Fertility in patients with chronic illnesses is often decreased in part due to ED,
ejaculatory disorders and infection of the lower urinary & genital tract. For patients with
ejaculatory problems, sperm can be harvested by post orgasm urine or electro-ejaculation.
Sperm can also be harvested nowadays from the testes and kept in sperm bank. Modern
test tube baby techniques e.g. intracytoplasmic sperm injection (ISCI) can help many
subfertile couples.
SUMMARY:
ED is seen in about 60% of patients with chronic renal failure. Specific treatment with
PDE-5 I is effective in more than 60% of patients. ED should be treated early together
with the co-morbidities viz hypertension, diabetes, ischaemic heart disease,
dyslipidaemia, mental health and testosterone deficiency syndrome. Intra-penile
injection of vasodilators is useful in patients who do not respond to PDE-5 I.
NKF Annual Dialysis Meeting, Kuala Lumpur, 13th
December 2008
Monday, August 1, 2011
Damage only if op was done badly
SHRUNKEN-TESTICLES CASE ,
THE STRAITS TIMES: Sunday, August 26, 2000
SEVERE damage to both testicles could take place after surgery only if the operation
was done inappropriately or extremely badly, an expert witness from East Malaysia
said yesterday.
Dr Clarence Lei Chang Moh, 43, a consultant urologist who runs a specialist clinic in
Kuching, Sarawak, was testifying for the defence in the suit brought by American
cocoa trader Denis Matthew Harte, 36, against a Singapore consultant urologist and
Gleneagles Hospital.
Mr Harte is suing Dr Tan Hun Hoe, 46, and Gleneagles for medical negligence over
an alleged botched-up operation on April 28, 1997, which left him with shrunken
testicles.
Shortly after the operation, Mr Harte had a fall in the toilet and hit his head. The
next day, he complained of severe pain and a swollen scrotum. He saw Dr Tan again
only four days later, on May 2.
Dr Lei had said in his affidavit that varicocele ligation, the operation carried out, was
an accepted treatment to improve the general outcome for sub-fertility in men. He
felt that delay in diagnosing trauma to the testicles could cause them to shrink.
He added that it was his opinion that Dr Tan had done what a normal urologist would
have done in this region. He also found Dr Tan's standard of care to be adequate and
safe, he said.
He told the High Court yesterday that a man could experience swelling, significant
pain and collection of blood in the scrotum after such an operation.
Mr Edmund Kronenburg, one of the lawyers acting for Mr Harte, asked if a competent
surgeon should advise a patient of the risk of testicular atrophy. Dr Lei replied: "It is
exceedingly rare."
The lawyer suggested that it would be possible to get bilateral-testicular atrophy if
the surgery was inappropriately done. Dr Lei said: "It has to be a very, very
inappropriately-done surgery. You got to tie up all the arteries, all the veins. It has
to be a very, very bad surgery."
A Gleneagles staff nurse, Ms Looi Chai Hong, 57, and former nurse Tan Sang Eng,
45, who were on duty on the day of Mr Harte's operation, both testified they had not
found any injury on the site of Mr Harte's operation or any bruising to his scrotum
after his fall that day.
The hearing continues on Monday.
THE STRAITS TIMES: Sunday, August 26, 2000
SEVERE damage to both testicles could take place after surgery only if the operation
was done inappropriately or extremely badly, an expert witness from East Malaysia
said yesterday.
Dr Clarence Lei Chang Moh, 43, a consultant urologist who runs a specialist clinic in
Kuching, Sarawak, was testifying for the defence in the suit brought by American
cocoa trader Denis Matthew Harte, 36, against a Singapore consultant urologist and
Gleneagles Hospital.
Mr Harte is suing Dr Tan Hun Hoe, 46, and Gleneagles for medical negligence over
an alleged botched-up operation on April 28, 1997, which left him with shrunken
testicles.
Shortly after the operation, Mr Harte had a fall in the toilet and hit his head. The
next day, he complained of severe pain and a swollen scrotum. He saw Dr Tan again
only four days later, on May 2.
Dr Lei had said in his affidavit that varicocele ligation, the operation carried out, was
an accepted treatment to improve the general outcome for sub-fertility in men. He
felt that delay in diagnosing trauma to the testicles could cause them to shrink.
He added that it was his opinion that Dr Tan had done what a normal urologist would
have done in this region. He also found Dr Tan's standard of care to be adequate and
safe, he said.
He told the High Court yesterday that a man could experience swelling, significant
pain and collection of blood in the scrotum after such an operation.
Mr Edmund Kronenburg, one of the lawyers acting for Mr Harte, asked if a competent
surgeon should advise a patient of the risk of testicular atrophy. Dr Lei replied: "It is
exceedingly rare."
The lawyer suggested that it would be possible to get bilateral-testicular atrophy if
the surgery was inappropriately done. Dr Lei said: "It has to be a very, very
inappropriately-done surgery. You got to tie up all the arteries, all the veins. It has
to be a very, very bad surgery."
A Gleneagles staff nurse, Ms Looi Chai Hong, 57, and former nurse Tan Sang Eng,
45, who were on duty on the day of Mr Harte's operation, both testified they had not
found any injury on the site of Mr Harte's operation or any bruising to his scrotum
after his fall that day.
The hearing continues on Monday.
Wednesday, July 20, 2011
Over Active Bladder膀胱問題
Bph case studies 10.7.11 dr lei
View more presentations from Wong Lei.
Oab cases(1)
View more presentations from Wong Lei.
Oab diagnosis & evaluation
View more presentations from Wong Lei.
Oab medical management
View more presentations from Wong Lei.
Tuesday, July 12, 2011
Wednesday, July 6, 2011
THE ROADs NOT TAKEN
Brain-drain (or recently brain-gain) used to be an important part of life. When I
graduated as a doctor, there were not many opportunities for specialised training. I
considered going to:-
(1)Singapore – Upon graduation, half of my classmates from Sarawak did their
housemanship in Singapore Singapore
get specialised training. A few succeeded but have to stay behind because their
spouses would not return to Malaysia
train “foreigners” in Singapore
my obligation to return to Sarawak .
(2) Australia – In 1988, I was offered a 1-2 years’ job in Perth
This was made possible because a Malaysian who had graduated as a urologist
by training in Malaysia had migrated to Perth
decided that I should only receive half of the pay of an Australian registrar. I would
also not be eligible to sit for the FRACS Urology exam.
Needless to say, I did not take up “compromised” offer.
(3) USA – At the same time, I considered training in the USA
have the world’s most advanced medical centres. To do that, I passed the ECFMG
exam (Examination Conducted for Foreign Medical Graduates). The residency
programme in the US
years. There would be therefore the chance that I would not be able to complete my
training if I do not get a 1 year extension.
(4) United Kingdom
namely, a candidate was awarded a scholarship but committed suicide thereafter),
I was able to fight for a scholarship to do Urology in the United Kingdom
spending 2 years, namely, at the University of London and University of Edinburgh
I returned to Malaysia
of the University of Edinburgh
consultant urologist at the Western General Hospital
ends meet and also in the cold dam weather. I also had a 2 year bond with the
Malaysian Government, just having utilised their scholarship. I therefore declined the
faxed letter of offer from the late Professor Chisholm who was my main mentor when
I was in Edinburgh
However, in the current globalised world, it does not really matter where I stay and also
at this age.
Dr Clarence Lei Chang Moh
Date: 4th July 2011
Sunday, July 3, 2011
MEN’S HEALTH: Hormonal Replacement Therapy更換荷爾蒙治療法(HRT)
Male menopause do occur although it manifests in a insidious manner and it is also not
as common as in females. Medical guidelines have been published, e.g. in European
Urology 2005 Volume 48, Page 1 – 4. There are other terminology used for this
condition, namely, Andropause, ADAM or Androgen Deficiency in Aging Male, PADAM,
Partial Androgen Deficiency in Aging Male, LOH or Late Onset Hypogonadism. The
latest description is that of TDS, Testosterone Deficiency Syndrome. The various
names illustrates that there is probably no sharp drop in the testosterone level but rather
a gradual decrease in level. In addition, there is often a variation in individual level as
well as a wide variation among the population of the level of male hormone. There is
probably also a normal natural decline of the male hormone with graceful aging. Other
hormonal replacements are still undergoing trials.
DEFINITION:
The definition of male menopause would be that of a “clinical and biochemical condition
associated with aging male”.
The clinical features would include decreased libido, erectile dysfunction (ED), sleep
disturbances, changes in mental status e.g. irritability, tiredness and poor memory.
There may also be bodily changes e.g. increase in visceral fat, decrease in lean body
mass and osteoporosis.
The scientific measurement is that of the blood total testosterone determination taken in
the morning between 7 – 11 am. The current lower limit of total testosterone is that of
<11 ng/L.
ASSOCIATED CO-MORBIDITY:
There are some conditions which are associated with an increased incidence of
TDS and these include diabetes, hypertension, obesity (waist circumference >90
cm for Asians), osteoporosis and dyslipidaemia. Some group these conditions as
the “metabolic syndrome”.
Precautions before starting on testosterone replacement therapy include exclusion of
prostatic cancer. The growth of prostate cancer depends on testosterone. Therefore,
before the initiation of testosterone replacement therapy, one would need to do an
examination of the prostate, usually a digital rectal examination, DRE and also to
measure the blood level for prostatic specific antigen, PSA. However, prostatic cancer
is extremely common and testosterone replacement therapy is only contraindicated in
patients with a clinically active prostate cancer. Testosterone replacement therapy in
men with untreated subclinical prostate cancer is not associated with prostate cancer
progression in the short to middle term of a few years (Journal of Urology 2011; Vol.
185: 1256-1261).
WHICH HORMONAL PREPARATION TO USE?
There have been many preparations used over the years including tablets, creams and
injections. The aim is to have testosterone replacement therapy, not to give supra-
physiological levels. Orally absorbed testosterone will have to pass through the liver,
2
giving rise to liver toxicity. In addition, there is a question of compliance when the
patient has to take the capsules, usually twice a day. There are also some gels which
can be applied to the skin, in an attempt to mimic the diurnal rhythm of the normal
testosterone. In humid hot climate, gels may not be comfortable. Previously, there were
injections but these tend to give supra-physiological levels during the early days of the
injections. Moreover, many of these preparations were short acting, usually for about 3
weeks.
Obviously, injection therapy which can give a sustained replacement dose over a period
of months would be the most suitable formulation. One such formulation is that of
injection Nebido. This can be given every 3 monthly, although an earlier second dose
would be needed (usually at 6 weeks) to top up the testosterone level.
FOLLOW-UP:
Testosterone replacement therapy is an expensive medical treatment. Therefore,
patients should follow up with their doctor to review their progress including a prostatic
evaluation on an annual basis.
Dr Clarence Lei Chang Moh
Consultant Urologist
Enquries to : clarencelei@gmail.com
kuchingurology.com
Date: 15.6.2011
as common as in females. Medical guidelines have been published, e.g. in European
Urology 2005 Volume 48, Page 1 – 4. There are other terminology used for this
condition, namely, Andropause, ADAM or Androgen Deficiency in Aging Male, PADAM,
Partial Androgen Deficiency in Aging Male, LOH or Late Onset Hypogonadism. The
latest description is that of TDS, Testosterone Deficiency Syndrome. The various
names illustrates that there is probably no sharp drop in the testosterone level but rather
a gradual decrease in level. In addition, there is often a variation in individual level as
well as a wide variation among the population of the level of male hormone. There is
probably also a normal natural decline of the male hormone with graceful aging. Other
hormonal replacements are still undergoing trials.
DEFINITION:
The definition of male menopause would be that of a “clinical and biochemical condition
associated with aging male”.
The clinical features would include decreased libido, erectile dysfunction (ED), sleep
disturbances, changes in mental status e.g. irritability, tiredness and poor memory.
There may also be bodily changes e.g. increase in visceral fat, decrease in lean body
mass and osteoporosis.
The scientific measurement is that of the blood total testosterone determination taken in
the morning between 7 – 11 am. The current lower limit of total testosterone is that of
<11 ng/L.
ASSOCIATED CO-MORBIDITY:
There are some conditions which are associated with an increased incidence of
TDS and these include diabetes, hypertension, obesity (waist circumference >90
cm for Asians), osteoporosis and dyslipidaemia. Some group these conditions as
the “metabolic syndrome”.
Precautions before starting on testosterone replacement therapy include exclusion of
prostatic cancer. The growth of prostate cancer depends on testosterone. Therefore,
before the initiation of testosterone replacement therapy, one would need to do an
examination of the prostate, usually a digital rectal examination, DRE and also to
measure the blood level for prostatic specific antigen, PSA. However, prostatic cancer
is extremely common and testosterone replacement therapy is only contraindicated in
patients with a clinically active prostate cancer. Testosterone replacement therapy in
men with untreated subclinical prostate cancer is not associated with prostate cancer
progression in the short to middle term of a few years (Journal of Urology 2011; Vol.
185: 1256-1261).
WHICH HORMONAL PREPARATION TO USE?
There have been many preparations used over the years including tablets, creams and
injections. The aim is to have testosterone replacement therapy, not to give supra-
physiological levels. Orally absorbed testosterone will have to pass through the liver,
2
giving rise to liver toxicity. In addition, there is a question of compliance when the
patient has to take the capsules, usually twice a day. There are also some gels which
can be applied to the skin, in an attempt to mimic the diurnal rhythm of the normal
testosterone. In humid hot climate, gels may not be comfortable. Previously, there were
injections but these tend to give supra-physiological levels during the early days of the
injections. Moreover, many of these preparations were short acting, usually for about 3
weeks.
Obviously, injection therapy which can give a sustained replacement dose over a period
of months would be the most suitable formulation. One such formulation is that of
injection Nebido. This can be given every 3 monthly, although an earlier second dose
would be needed (usually at 6 weeks) to top up the testosterone level.
FOLLOW-UP:
Testosterone replacement therapy is an expensive medical treatment. Therefore,
patients should follow up with their doctor to review their progress including a prostatic
evaluation on an annual basis.
Dr Clarence Lei Chang Moh
Consultant Urologist
Enquries to : clarencelei@gmail.com
kuchingurology.com
Date: 15.6.2011
Wednesday, June 15, 2011
PAEDIATRIC RENAL TRANSPLANTATION馬來西亞腎臟移植
PAEDIATRIC RENAL TRANSPLANTATION IN MALAYSIA
CCM Lei, Koh ET, Murali S, Susan W, Yap YC, Lim YN
Institute of Urology & Nephrology, Hospital Kuala Lumpur
The first kidney transplant in Malaysia was done on 15th December 1975 with a living related kidney from his younger brother. The patient and kidney survived till 26.3.2006 when the patient died with a functioning kidney. The first cadaveric kidney transplantation was done in Malaysia in 1979. The cadaveric transplant programme was re-activated on 22.7.1992 when a brain dead American lady donated both her kidneys, one of them going to an 11 year old paediatric recipient. Since then, the kidney transplant programme has remained stable, with an average of about 30 cases per year and more than one third of them from cadaveric sources.
With improved medical care by 10 paediatric nephrologists in Malaysia, there is an increasing number of paediatric kidney transplants. There are 25 children being worked up with a view to living related transplantation. Despite a good adult kidney transplantation programme, paediatric renal transplantation remains a formidable challenge, worldwide. All paediatric kidney transplantations in Malaysia are done at the Hospital Kuala Lumpur and the present review includes cases from 2000 to 2007. There are a total of 58 recipients, with 23 from live donors. The number of transplants are ( cadaveric in [ ] ): 2 [7] in 2000, 2 [2] in 2001; 3 [1] in 2002; 1 [3] in 2003; 1 [2] in 2004; 5 [2] in 2005; 3 [7] in 2006; 6 [11] in 2007). There were 3 mortality: 2 cadaveric (1 graft rupture and 1 non-functioning kidney) and 1 from a live donor who suffered severe pulmonary hypertension. There were 3 nephrectomies: 2 cadaveric and 1 living related graft which at ruptured 3 weeks postoperative. There were 3 significant surgical morbidity, namely, 2 perinephric haematomas which subsequently resolved and 1 aortoiliac renal artery false aneurysm which was repaired with the help of the vascular team. One recipient required cystoplasty (for posterior urethral valve) before receiving a cadaveric kidney, which was unfortunately lost because of thrombosis 2 weeks post transplant. Many paediatric patients are on CAPD. If there is primary function on table, the Tenchkoff is removed at the time of transplantation. Ureteric reimplantation is via extravesical submusoacl tunnel over a ureteric stent..
Infarction is a well known problem of paediatric transplants mainly because of a mis- match in blood flow of large donor kidney and small vessels. The larger vessels of external or common iliac are used for anastomosis. The internal iliac may be used to vascularise any accessory artery. In 10 cadaveric paediatric transplants in 2006, 4 of them had ischaemia and 2 required a graft nephrectomy. The other 6 kidneys have satisfactory renal function. Most paediatric recipients have a body weight >15 kg; 2 patients with body weight 10 to 15 kg were transplanted in deserving situations. Cadaveric donors less than 2 years old were extremely challenging and there were a total of 4 of them. Two sets were transplanted enbloc and both did not do well: one had bleeding, possibly associated with heparin on the 8th postoperative day and another kidney infarcted on the 10th postoperative day. The other set of small cadaveric kidneys were transplanted in 2 separate recipients and one patient died of unrelated chickenpox and the other kidney is functioning well. One set of cadaveric donors were transplanted into 1 recipient, 1 in each iliac fossa and both kidneys are functioning well.
All patients were closely followed by paediatric nephrologists throughout Malaysia. In addition to above vascular problems, 1 patient had exploration for wound haematoma, 1 lymphocele, 2 ATN requiring dialysis. One patient re-started CIC for hypoactive bladder. One had angioembolisation for bleeding after renal biopsy. Infection contributes to significant morbidity: UTIs in 9, CMV infection in 1, Herpes in 1, lung infection in 2. The patients were closely monitored with immunosuppression and for recurrent primary disease (2 cases of recurrent nephrotic, FSGS noted).
PAEDIATRIC RENAL TRANSPLANTATION
image taken from
Kidney stones (Renal calculi)腎結石
MEDICAL TREATMENT FOR RENAL CALCULI:
WHAT WORKS AND WHAT DON’T.
Dr Clarence Lei, FRCS Urol, Consultant Urologist, Stone Centre, NMSC
clarencelei@gmail.com
Urinary stones affects 5-15% of populations, with a 50% recurrence rate over 10 years. Ureteric colic is the most severe pain that men can ever experience and the standard treatment for most patients is that of Diclofenac. However, if this is given continuously for more than 48 hours, there is a nephrotoxic potential, especially in patients who are dehydrated. For small stones (< 6 mm) in the lower ureter, removal can be facilitated by uroselective alpha-blockers (e.g. Tamsulosin, Alfuzosin). This is now known as MET medical expulsive therapy! Stones <5mm usually do not require intervention unless complicated by sepsis whereas untreated large stones eventually cause urosepsis.
The important medical treatment for urinary stones is that of water therapy such that the patient produces 2 litres of urine per day. The fluid intake of the patient depends on his environment. Ideally, such fluid should be distributed throughout the day. There is no good evidence of advantages of specific juices or herbals.
Uric acid stones can be effectively dissolved by medical therapy by urinary alkalinisation, keeping the urine pH at 7.0. Uric acid stones comprise about 20% stones and are radiolucent on x-ray but readily seen on ultrasound and plain CT. Even staghorn uric acid calculi can be dissolved over 6 months. However, the patient should have a good renal function to avoid accumulation of the medications used e.g. potassium, citrate, sodium (in Ural).
Potassium Citrate helps clear post ESWL lower pole fragments (“stone free = <5mm”). In a study when Potassium Citrate was given as Urocit-K tablets 60 meq/day, Urocit-K increased the stone-free rate to 45.5% from 12.5% in control group, over a 12 month period. The citrate in the urine reduces crystallization of calcium and uric acid stones.
Stones associated with infection are called struvite stones. Struvite stones are typically soft and faintly radiolucent. The stone and infection should be cleared by surgery and vigorous antibiotic therapy (e.g. Amikacin) followed by prophylaxis e.g. Trimethoprim at night for 6 months, including in children.
For patients who have underlying metabolic effects, the benefit of the specific medications may not justify the side effects and long term costs. The diet recommendations for patients with recurrent stone formation is that of less salt, and normal calcium. Patients with uric acid stones should take less uric acid in their diet e.g. red meat, nuts.
Reference (more pdfs available on request): Singh SK et al. Medical therapy for calculus disease. Brit J Urol Int. 2011, 107: 356-368.;
Pak CYC Medical Stone Management: 35 yrs of advances. J Urol 2008, 180; 813 – 819.
Image taken from nursing crib.com
| http://nursingcrib.com/nursing-notes-reviewer/medical-surgical-nursing/renal-problems-%E2%80%93-renal-calculi/ |
Monday, June 13, 2011
CIRCUMCISION割包皮
CIRCUMCISION IN 2011
by Dr Clarence Lei Chang Moh, FRCS Urol
Consultant Urologist
INTRODUCTION:
I have been inspired to write on the above subject as it is “circumcision season during the current year-end school holidays”. The following situations are common.
§ Neonatal circumcision:
I get this request occasionally, mainly from expatriates from the Middle East. During the first week of life, the baby’s haematology is still protected by the mother and that would be the optimal time to do the circumcision. This can be done under a penile ring block with 1cc of 1% lignocaine solution injected with a 26G needle. 20% sucrose solution can be given to the child as a soothing agent during the circumcision
Jewish circumcision:
The Jewish circumcise within the first week of life. Jesus Christ was born as a Jew and his holy foreskin was said to be worshipped in at least 31 Western European churches! However, the Jews have their own trained personnel to conduct the circumcision and also to do the follow-up visits.
§ Ritual circumcision among the Malaysian Muslims:
The Muslims in Malaysia usually circumcise at puberty, during the school holidays when they finish school after standard 6. It is also a part of the culture of transition to manhood and therefore, many of these circumcisions are done as ritual in a very cost effective manner. They are usually done by trained medical personnel nowadays and most of the boys require only local anaesthetic. However, as the living pattern of some of the modern Muslims do not follow “kampung culture”, some of the boys are better circumcised under a general anaesthetic. In fact, I do see a number of “partially circumcised boys” who require a repeat circumcision as they were unable to cooperate with the procedure during the first circumcision!
§ Techniques of circumcision:
In 1992, a little boy had part of his penis sliced off by a hospital attendant in a government general hospital. He subsequently required corrective surgery including meatoplasty. There were also other similar incidences with medico-legal complications. The authorities recommended that the circumcision technique should therefore be that of a dorsal slit technique rather than a guillotine technique. I routinely use the dorsal slit technique with a pair of scissors and cut the inner and outer foreskin with a knife. The edges are then stitched with plain Catgut 4/0. I use an ocular loop (usually 4 x) and low setting bipolar diathermy for all my circumcisions.
The media sometimes advertise the use of “laser circumcision”. In fact, laser would have been an extremely expensive technology and I do not know of anybody using laser for circumcision! Various types of clamps have also been used for circumcision. Again, if one can make a clean incision and put a few stitches, the clamp is really rather cumbersome. If the skin edges are not sutured and if the clamp falls off prematurely, there will be a large gap and an ugly scar formed by secondary healing. Moreover, in bigger boys, the vessels could still bleed after the clamp drops off. If the patient requires a repeat circumcision, one would have to wait for more than a month to allow all the swelling and infection to settle down before the repeat circumcision.
§ Phimosis as an indication for circumcision:
In a small number of children, the prepuce opening might be very tight, causing obstruction to the urine flow. Typically, such a child would have ballooning of the prepuce at micturation and may be with some discomfort or crying. The following indicates ballooning of penis from phimosis.
Such patients are probably better off with a surgical circumcision. Circumcision is not covered by insurance policies, possibly because it is viewed as a cosmetic surgery or it is considered a congenital condition.
§
§ Medical treatment of paediatric phimosis:
Some parents may be against a circumcision. Moreover, the patient may not be fit for circumcision. In such a milder case of phimosis, the foreskin can be softened with a daily application of a steroid cream (e.g. Dermovate) and retracting the foreskin gently at each bath. This may have to be done for a month or so and some of the phimosis will still recur.
Late onset adult phimosis:
This can cause voiding difficulties and infection. Up to 1/3 of these patients have underlying diabetes mellitus and therefore must be screened as such. It can also happen in old folks’ homes where nobody cleans the penis.
§ Other common medical indications for circumcision:
If the prepuce is retracted and not replaced, it can strangulate the glans penis, giving rise to a condition called “Paraphimosis”. It is not uncommon in young boys who “play with their prepuce” or in elderly men who have the prepuce retracted (e.g. by the nurse while cleaning the penis for urethral catheterisation) and the prepuce is not replaced. A little boy who was apparently turned away by the doctor who did not diagnose the paraphimois:
Another common indication for circumcision is that of infection of the glans penis and prepuce (a condition called Balanoposthitis).
A common indication is that it is “a good hygiene” to have a circumcision. Unfortunately, this gives the implication that men who are not circumcised do not clean their penis and foreskin!
Is there any contraindication for circumcision?
The absolute contraindications for circumcision are:
(1) Hypospadias, where the urethral opening is proximal. The foreskin is often used by the urologist to do surgical correction for the hypospadias.
(2) Any other underlying medical disorder e.g. haemophilia.
What is the relationship between male circumcision and urinary tract infection, UTI?
For male children who have recurrent febrile UTI, circumcision has a beneficial effect. For patients with high grade vesico-ureteric reflux, circumcised children have less kidney scars (10.2% compared to 5.2%, J. Urol 2010, 184: 1598-1603). Such high grade reflux often also occurs in a condition affecting male infants, namely that of PUV, posterior urethral valve. These are some of the common medical indications for circumcision in children.
What are the community indications for circumcision?
(1) It has been known for a long time that circumcision confers a beneficial effect in terms of cancer of the penis. The Jews who are circumcised soon after birth do not develop cancer of the penis. The Muslims who are circumcised at puberty have a less incidence of cancer of penis.
(2) It had been shown that the circumcised men in sub-Saharan Africa have less HIV/AIDS (BJUI 2008: 101, 394). The WHO is leading a campaign for circumcision in these areas.
(3) It had also been shown male circumcision confers a beneficial effect for penile HPV infection and also reduce cervical cancer in their female partners (NEJM 2002; 346: 1105-1112).
§ The role of circumcision and penile size:
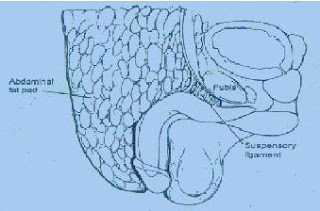
Many anxious mothers bring their obese boys to consider circumcision, thinking that the prepuce covers the penis. Micropenis is indeed an extremely rare condition. Most of the time, the penis is actually retracted and hidden underneath the pubic fat! If the doctor does an aggressive circumcision, he may end up removing too much penile skin and the penis does not even come to the surface. The size of the penis cans usually be shown to the mother by lying the patient down and putting pressure on the suprapubic fat to expose the penis!
The following diagram illustrates the problem of childhood obesity and the “redundant foreskin”.
“Buried Penis”:
In rare cases, the penile skin is insufficient and prevents the penis from growing at puberty. In such cases, the foreskin can be retracted and tacked down to penis by suture as below:
Postoperative care of circumcision:
The postoperative wound actually does not require any dressing except for wound inspection and reassurance of the parents. Topical ointment e.g. Chloramphenicol eye ointment may be applied on a daily basis to reduce adhesions to the garments. A lot of Muslim boys would just leave the penis “exposed” by wearing a loose sarung. If there is any oozing, a circumferential light pressure dressing may help. The wound can be inspected every few days and the child can probably have a bath after a week or so. I would recommend avoiding long distant travel for about 2 weeks. For men, bleeding can occur during an erection and therefore, I would recommend sexual abstinence for a month.
§ How much foreskin to remove?
If one removes too much skin, there may be insufficient skin for free erection. However, if not enough skin is removed, the sulcus and the glans penis are not exposed and the patient may require re-circumcision!
§ Uncircumcision:
There is a group of believers that the prepuce is an important part of the human anatomy and extremely rich in nerve endings. Therefore, some communities do not wish to have circumcision and those who are circumcised at birth would have their circumcision revised by an uncircumcision operation. However, the prepuce probably plays a small part in overall sexual pleasure and a recent study showed no such difference (BJUI 2008; 101: 65-70).
Dr Clarence Lei Chang Moh,
clarencelei@gmail.com
Subscribe to:
Comments (Atom)