CIRCUMCISION IN 2011
by Dr Clarence Lei Chang Moh, FRCS Urol
Consultant Urologist
INTRODUCTION:
I have been inspired to write on the above subject as it is “circumcision season during the current year-end school holidays”. The following situations are common.
§ Neonatal circumcision:
I get this request occasionally, mainly from expatriates from the Middle East. During the first week of life, the baby’s haematology is still protected by the mother and that would be the optimal time to do the circumcision. This can be done under a penile ring block with 1cc of 1% lignocaine solution injected with a 26G needle. 20% sucrose solution can be given to the child as a soothing agent during the circumcision
Jewish circumcision:
The Jewish circumcise within the first week of life. Jesus Christ was born as a Jew and his holy foreskin was said to be worshipped in at least 31 Western European churches! However, the Jews have their own trained personnel to conduct the circumcision and also to do the follow-up visits.
§ Ritual circumcision among the Malaysian Muslims:
The Muslims in Malaysia usually circumcise at puberty, during the school holidays when they finish school after standard 6. It is also a part of the culture of transition to manhood and therefore, many of these circumcisions are done as ritual in a very cost effective manner. They are usually done by trained medical personnel nowadays and most of the boys require only local anaesthetic. However, as the living pattern of some of the modern Muslims do not follow “kampung culture”, some of the boys are better circumcised under a general anaesthetic. In fact, I do see a number of “partially circumcised boys” who require a repeat circumcision as they were unable to cooperate with the procedure during the first circumcision!
§ Techniques of circumcision:
In 1992, a little boy had part of his penis sliced off by a hospital attendant in a government general hospital. He subsequently required corrective surgery including meatoplasty. There were also other similar incidences with medico-legal complications. The authorities recommended that the circumcision technique should therefore be that of a dorsal slit technique rather than a guillotine technique. I routinely use the dorsal slit technique with a pair of scissors and cut the inner and outer foreskin with a knife. The edges are then stitched with plain Catgut 4/0. I use an ocular loop (usually 4 x) and low setting bipolar diathermy for all my circumcisions.
The media sometimes advertise the use of “laser circumcision”. In fact, laser would have been an extremely expensive technology and I do not know of anybody using laser for circumcision! Various types of clamps have also been used for circumcision. Again, if one can make a clean incision and put a few stitches, the clamp is really rather cumbersome. If the skin edges are not sutured and if the clamp falls off prematurely, there will be a large gap and an ugly scar formed by secondary healing. Moreover, in bigger boys, the vessels could still bleed after the clamp drops off. If the patient requires a repeat circumcision, one would have to wait for more than a month to allow all the swelling and infection to settle down before the repeat circumcision.
§ Phimosis as an indication for circumcision:
In a small number of children, the prepuce opening might be very tight, causing obstruction to the urine flow. Typically, such a child would have ballooning of the prepuce at micturation and may be with some discomfort or crying. The following indicates ballooning of penis from phimosis.
Such patients are probably better off with a surgical circumcision. Circumcision is not covered by insurance policies, possibly because it is viewed as a cosmetic surgery or it is considered a congenital condition.
§
§ Medical treatment of paediatric phimosis:
Some parents may be against a circumcision. Moreover, the patient may not be fit for circumcision. In such a milder case of phimosis, the foreskin can be softened with a daily application of a steroid cream (e.g. Dermovate) and retracting the foreskin gently at each bath. This may have to be done for a month or so and some of the phimosis will still recur.
Late onset adult phimosis:
This can cause voiding difficulties and infection. Up to 1/3 of these patients have underlying diabetes mellitus and therefore must be screened as such. It can also happen in old folks’ homes where nobody cleans the penis.
§ Other common medical indications for circumcision:
If the prepuce is retracted and not replaced, it can strangulate the glans penis, giving rise to a condition called “Paraphimosis”. It is not uncommon in young boys who “play with their prepuce” or in elderly men who have the prepuce retracted (e.g. by the nurse while cleaning the penis for urethral catheterisation) and the prepuce is not replaced. A little boy who was apparently turned away by the doctor who did not diagnose the paraphimois:
Another common indication for circumcision is that of infection of the glans penis and prepuce (a condition called Balanoposthitis).
A common indication is that it is “a good hygiene” to have a circumcision. Unfortunately, this gives the implication that men who are not circumcised do not clean their penis and foreskin!
Is there any contraindication for circumcision?
The absolute contraindications for circumcision are:
(1) Hypospadias, where the urethral opening is proximal. The foreskin is often used by the urologist to do surgical correction for the hypospadias.
(2) Any other underlying medical disorder e.g. haemophilia.
What is the relationship between male circumcision and urinary tract infection, UTI?
For male children who have recurrent febrile UTI, circumcision has a beneficial effect. For patients with high grade vesico-ureteric reflux, circumcised children have less kidney scars (10.2% compared to 5.2%, J. Urol 2010, 184: 1598-1603). Such high grade reflux often also occurs in a condition affecting male infants, namely that of PUV, posterior urethral valve. These are some of the common medical indications for circumcision in children.
What are the community indications for circumcision?
(1) It has been known for a long time that circumcision confers a beneficial effect in terms of cancer of the penis. The Jews who are circumcised soon after birth do not develop cancer of the penis. The Muslims who are circumcised at puberty have a less incidence of cancer of penis.
(2) It had been shown that the circumcised men in sub-Saharan Africa have less HIV/AIDS (BJUI 2008: 101, 394). The WHO is leading a campaign for circumcision in these areas.
(3) It had also been shown male circumcision confers a beneficial effect for penile HPV infection and also reduce cervical cancer in their female partners (NEJM 2002; 346: 1105-1112).
§ The role of circumcision and penile size:
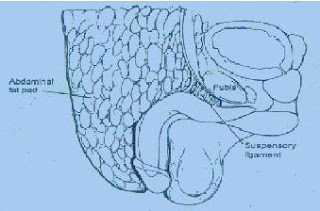
Many anxious mothers bring their obese boys to consider circumcision, thinking that the prepuce covers the penis. Micropenis is indeed an extremely rare condition. Most of the time, the penis is actually retracted and hidden underneath the pubic fat! If the doctor does an aggressive circumcision, he may end up removing too much penile skin and the penis does not even come to the surface. The size of the penis cans usually be shown to the mother by lying the patient down and putting pressure on the suprapubic fat to expose the penis!
The following diagram illustrates the problem of childhood obesity and the “redundant foreskin”.
“Buried Penis”:
In rare cases, the penile skin is insufficient and prevents the penis from growing at puberty. In such cases, the foreskin can be retracted and tacked down to penis by suture as below:
Postoperative care of circumcision:
The postoperative wound actually does not require any dressing except for wound inspection and reassurance of the parents. Topical ointment e.g. Chloramphenicol eye ointment may be applied on a daily basis to reduce adhesions to the garments. A lot of Muslim boys would just leave the penis “exposed” by wearing a loose sarung. If there is any oozing, a circumferential light pressure dressing may help. The wound can be inspected every few days and the child can probably have a bath after a week or so. I would recommend avoiding long distant travel for about 2 weeks. For men, bleeding can occur during an erection and therefore, I would recommend sexual abstinence for a month.
§ How much foreskin to remove?
If one removes too much skin, there may be insufficient skin for free erection. However, if not enough skin is removed, the sulcus and the glans penis are not exposed and the patient may require re-circumcision!
§ Uncircumcision:
There is a group of believers that the prepuce is an important part of the human anatomy and extremely rich in nerve endings. Therefore, some communities do not wish to have circumcision and those who are circumcised at birth would have their circumcision revised by an uncircumcision operation. However, the prepuce probably plays a small part in overall sexual pleasure and a recent study showed no such difference (BJUI 2008; 101: 65-70).
Dr Clarence Lei Chang Moh,
clarencelei@gmail.com