PROSTATE CANCER SCREENING: Pros and Cons
By Dr Clarence Lei, FRCS Urol, FEBU, Consultant Urologist
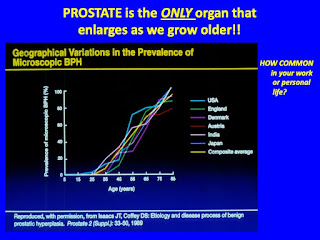
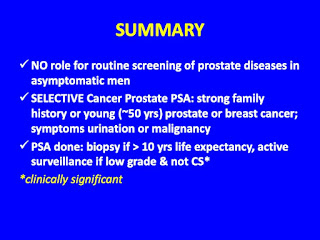
Prostate gland is the organ giving rise to the most morbidities in men after the age of 50. Most of the prostatic diseases are of benign nature, although 20% of prostatic concerns are cancerous. About 50-90% of prostatic cancers in developing countries are in an advanced stage at presentation. Since the early 1990s, the urology community has been debating regarding the cost effectiveness of screening for prostate cancer.
Prostate cancer is a cancer that almost all men will get if they live long enough. In 2016, cancer is the 4thleading cause of death, contributing to 12.6% of all deaths in Malaysian government hospitals; prostate cancer is only the 12thon the list. Prostate cancer is usually a slow growing cancer and indeed, the 5 year survival of all prostate cancer for Malaysia from the period 2007 to 2011 is 73.6%. Therefore, we have to balance the risks and benefits of screening for prostate cancer.
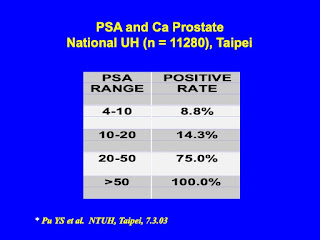
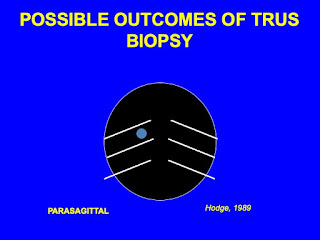
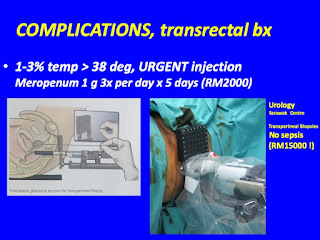
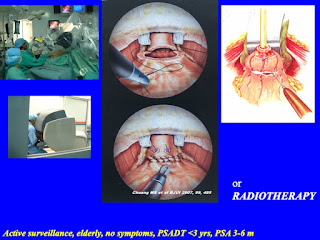
Doing a PSA, prostatic specific antigen is simple enough. But prostate cancer needs to be diagnosed with further imaging (specialised multi-parametric MRI being the latest tool) and usually with transrectal ultrasound guided systemic and targeted needle biopsies. The main complication of these biopsies is that of severe sepsis. If organ confined prostate cancer is diagnosed, a standard treatment is that of RARP, robot assisted radical prostatectomy. However, this is an expensive procedure; probably about RM100,000 in private. The main risks are those of sexual dysfunction in most cases and up to 5% of them will have permanent incontinence.
In primary care, most patients would already have a PSA, prostatic specific antigen done. It is challenge for the primary doctor to determine which patients will benefit from further investigation and not to miss out the clinically significant (CS) prostate cancer!
22ndFamily Medicine Scientific Conference, Kuching
3 August 2019